By John M. Norian, MD FACOG Reproductive Endocrinology and Infertility
Recurrent Pregnancy Loss: The Basics
Miscarriage is far more common than most people think. One in every four clinically-recognized pregnancies is lost in the first trimester. Overall, the rate of miscarriages rises with increasing maternal age. A spontaneous abortion or miscarriage is defined as loss of a pregnancy before 20 gestational weeks. The American Society for Reproductive Medicine (ASRM) recommends that couples who have two or more spontaneous miscarriages warrant an evaluation.
Recurrent pregnancy losses (RPLs) affect upwards of 5% of couples who achieve pregnancy and is defined by
the ASRM as two or more failed pregnancies documented by ultrasound or histopathology. Pregnancy loss exacts an immense psychological toll on affected couples and increased sensitivity and emotional support during follow-up evaluations and during ensuing pregnancies is warranted and may improve outcomes as documented in non-randomized studies.
Successful Pregnancy Rates in Idiopathic RPL
Current investigations and treatments allow physicians to identify treatable etiologies and to prevent certain recurrences. In couples with unexplained RPL, a large percentage of couples stratified by different ages will have subsequent live births even after two, three, four, or five prior miscarriages (see Figure above).
RPL: Etiology and Treatment
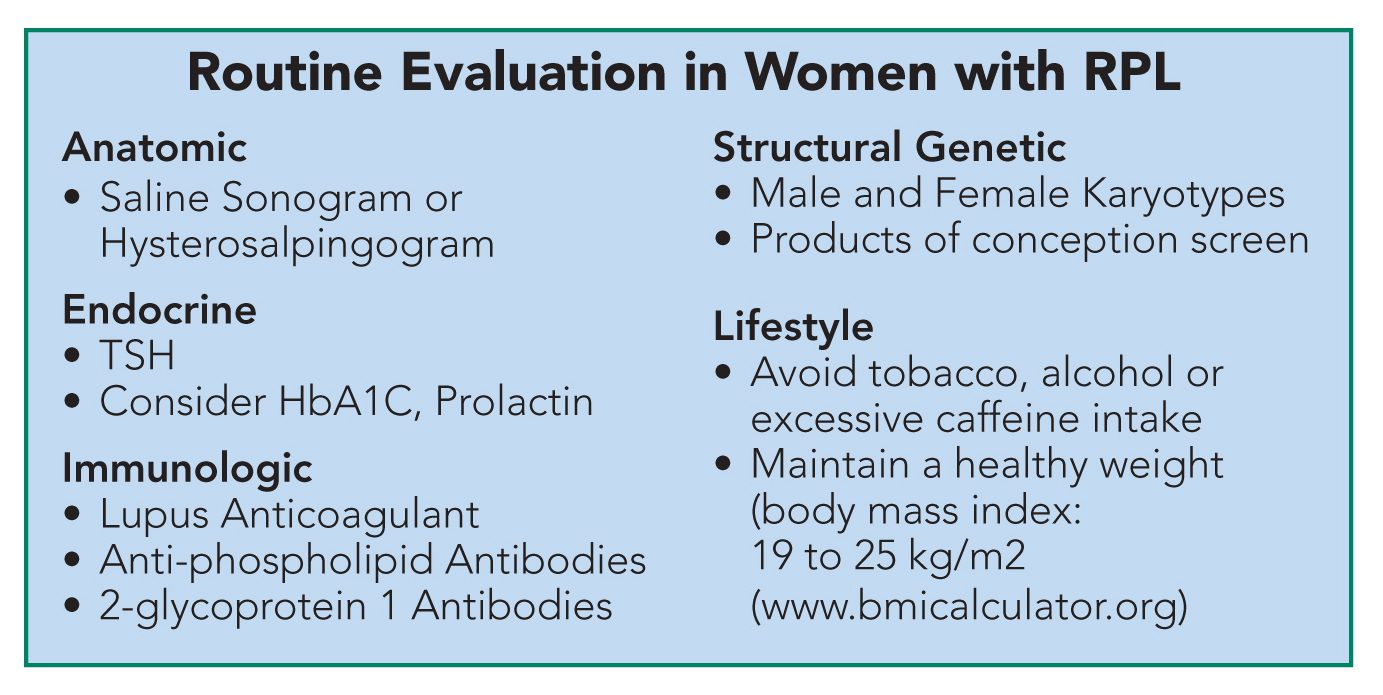
Common etiologies of recurrent miscarriages include genetic, anatomic, endocrinologic, immunologic, psychologic or lifestyle-related (see Table below). Many of these can be treated depending upon the cause, i.e., levothyroxine for those with hypothyroidism or pre-implantation genetic diagnosis can assist couples
with certain chromosomal translocations.
The use of heparin and low-dose aspirin is no-longer recommended for patients with unexplained RPL.
However, in patients with immune-mediated RPL (e.g., anti-phospholipid syndrome), unfractionated heparin with low-dose aspirin has demonstrated benefit, whereas studies with low-molecular weight heparin are conflicting. This is likely explained through unfractionated heparin’s immune effects in addition to its anti-thrombotic mechanism of action.
Routine screening for inherited thrombophilias is no longer indicated. However, screening (specifically for factor V Leiden and the prothrombin gene mutations, protein C, protein S, and antithrombin deficiencies) may be clinically justified when a patient has a personal history of venous thromboembolism or a first-degree relative with a known high-risk thrombophilia.
|
Etiology |
Percentage with |
|
Cytogenetic |
3% – 5% |
|
Anatomic |
15% – 20% |
|
Endocrinologic |
8% – 12% |
|
Immunologic |
15% – 20% |
|
Lifestyle |
Unknown* |
|
Psychologic |
Unknown** |
|
Unexplained |
40% – 50% |
* Cigarette smoking, alcohol consumption (three to five drinks per week), increased caffeine consumption (>3 cups of coffee), cocaine use, and obesity (body mass index >30 kg/m2 (www.bmicalculator.org) are associated with increased RPL.
**An association between psychological stress and RPL likely exists although the precise percentage of cases is not known.
The hormonal environment for the developing fetus is important. Miscarriage rates are higher in women with
sub-clinical hypothyroidism (elevated TSH, but normal free T4), hyperprolactinemia, uncontrolled diabetes, and also in women with polycystic ovarian syndrome (PCOS). Corresponding treatment with levothyroxine or a dopamine agonist (eg., bromocriptine or cabergoline) or weight loss and metformin improves subsequent pregnancy outcomes.
Large clinical trials demonstrating efficacy for progesterone treatment in RPL are lacking. In women with unexplained RPL there may be benefit (200 mg three times daily); however, the meta-analyses include less 140 patients. There were no differences in outcomes between the routes of administration of progesterone therapy (i.e., vaginal or intramuscular).
New Technology: Fetal Assessment and Pre-Genetic Screening
Performing chromosomal testing on the products of conception (POC) during a miscarriage can assist with diagnosis, avoid further testing, and may also be of psychological value to the couple. Recent advances in technology are more specific and can easily screen for maternal cell contamination.
Using a microchip [such as either a single nucleotide polymorphism (SNP) array or array comparative genomic hybridization (aCGH)], the POCs can be screened very specifically. This technology detects different types of aneuploidy (extra or missing chromosomes and also deletions or duplications) more precisely than traditional karyotyping. The result is typically available within two days. Failure to obtain a result is low (less than 1% of submitted specimens) (www.natera.com or www.reprogenetics.com). A large retrospective cost-effectiveness study of four UK centers concluded that the routine karyotyping of couples with recurrent miscarriage should be limited to those patients with unbalanced translocations in the POC.
When one of the partners has a structural genetic abnormality (e.g., a balanced chromosomal translocation), pre-genetic screening (PGS) or amniocentesis are options to detect the genetic abnormality in the offspring. Whether PGS of the embryos created through assisted reproductive technology decreases miscarriages in patients with RPL and a structural genetic abnormality is controversial. Newer methods of PGS may help better select embryos and decrease RPL in select patients.
Screening the Products of Conception Using New Hybridization Platforms (either SNP array or array CHG)
References
Practice Committee of the American Society for Reproductive Medicine, Evaluation and treatment of recurrent pregnancy loss: a committee opinion, Fertil Steril 2012; 98 (5): 1103-11.
Stray-Pedersen B, Stray Pedersen S. Recurrent abortion: the role of psychotherapy. In: Beard RW, ShipF, editors. Early pregnancy loss: mechanisms and treatment. New York: Springer-Verlag; 1988:433-40.
Brigham SA, Conlon C, Farquharson RG. A longitudinal study of pregnancy outcome following idiopathic recurrent miscarriage. Hum Reprod 1999; 14(1): 2868-71.
Branch DW, Gibson M, Silver RM. Clinical practice, recurrent miscarriage. New Engl Journ Med 2010; 363(18): 1740-7.
Kutteh WH, Odom LH. Evaluating recurrent pregnancy loss: the role of autoimmunity screening. Sexuality, Reproduction, Menopause. 2012; 10(1):5-11.
Haas DM, Ramsey PS. Progestogen for preventing miscarriage. Cochrane Database Sys Rev 2008; 16(2): CD003511.
Forman EJ, Tao X, Ferry KM, Taylor D, Treff NR, Scott RT Jr. Single embryo transfer with comprehensive chromosome screening results in improved ongoing pregnancy rates and decreased miscarriage rates. Hum Reprod 2012; 27(4): 1217-22.

